

By Monica Bolbjerg, MD, co-founder and CEO of Qure4u
Healthcare has been flirting with Remote Patient Monitoring (RPM) for a decade, and in theory RPM makes so much sense. So, why aren’t we seeing RPM being rolled out at scale?
Having worked with RPM since it first appeared on the healthcare map, I believe we’re on the verge of a breakthrough as the devices become more reliable and data-flow more precise and stable.
This playbook is meant to help you put together an RPM plan so you can scale quickly and enjoy early success.
Step 1: Define your goal
Your RPM program can look pretty different depending on your goal, and you might even put together several programs to achieve different goals.
Is your goal to …
Once your goal is defined, you need to build your program.
Step 2: Build a successful RPM program
Pick an initial use case/condition that is:
Don’t start with rare conditions. You want enough patients to get early momentum as you learn the best way to talk to your patients about the program.
Don’t go cheap! You want a cellular-enabled device that allows data to flow directly to your RPM platform. These devices are not the cheapest, but you’ll benefit from not having to pay staff to onboard patients or troubleshoot connection problems. Another bonus: Your patients will stay longer in the program thanks to minimal (or no) technology challenges for them.
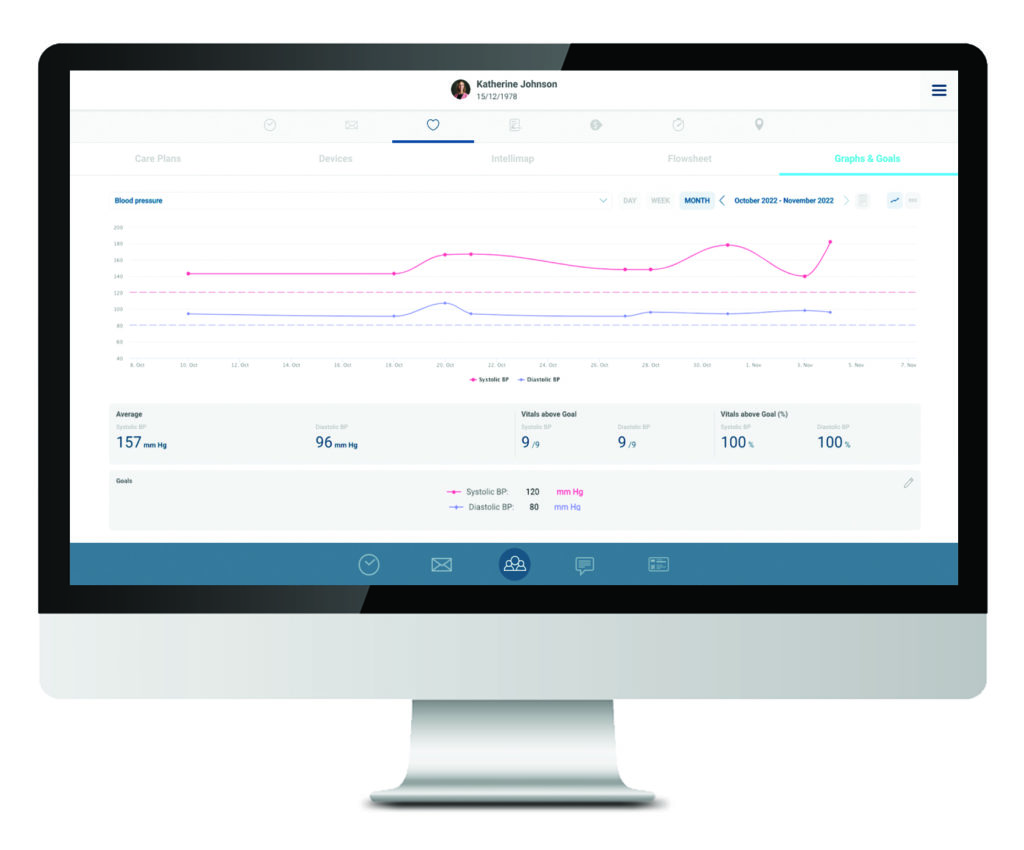
You will need an RPM management platform integrated to your EHR because EHRs are not built for the volume of data you will receive once you go live with home-monitoring devices for your patients.
The RPM platform should:
Maybe most importantly, make sure the RPM platform you choose can show the care coordinator lists of patients who have vitals out-of-range or are non-compliant. You don’t want your staff reviewing data for every patient every day.
Preferably, the RPM platform you choose includes device ordering and management. Today, you can order devices directly from the platform with a click of a button, and the device is shipped directly to the patient’s home.
This means you no longer need to pre-buy devices in bulk. This saves you cash and:
Not all patients “get it” right away, so to effectively onboard patients, you need to “sell it” to them. What’s in it for the patients? How much work is it?
Try these ideas:
Now you’re almost ready to get started. You probably have some providers who are more eager than others … so begin with them. But take note: When possible, choose more than a handful of providers for the launch of this project, because if they run into barriers, get distracted, or give up, it might look as if the entire thing is a failure, when it’s not. Challenges are inevitable, so embrace the early setbacks because this gives you the opportunity to figure things out before you do it at scale.
As you create a pitch for your patients, you’ll also need to “sell it” to your providers and nurses. I recommend creating an internal FAQ and good training of internal workflows.
One of the biggest mistakes organizations make, in my opinion, is to begin their RPM program with the sickest patients.
I get it. It would be amazing if providing an RPM device could help that population, but the sickest patients typically have 2-3 conditions, are on multiple medications, and need much more than home-monitoring to get better. They’re also often not tech-savvy because many of them are elderly, and you don’t want to spend more resources supporting them with RPM devices than if you simply keep them on your current treatment program.
Successful programs typically start with patients who have only one condition and are motivated to get better. That might be 30-50% of the patients in your targeted demographic, and because this population often requires less staff attention, your staff is free to onboard the more “complex” patients next.
Another benefit of starting with the “easy” or “simple” patients is that you’ll probably get great success stories that can be shared with other patients to help them get started.
Choose one condition with one or two vitals to measure, define one initial goal that is achievable within three months, evaluate, adjust, and set a new three-months goal.
Good luck and please share back your experiences and feedback.
Together, we’re reinventing what’s possible in healthcare.
Qure4u Inc. 2024